
Diet and Inflammation
Chronic systemic inflammation is implicated in the development of numerous chronic diseases, including cancer, cardiovascular disease, diabetes, respiratory and musculoskeletal disorders as well as adverse mental health outcomes.
Diet and inflammation
Diet can modulate inflammation, with some foods and nutrients having anti-inflammatory effects (such as phytochemicals from fruits and vegetables) and others having pro-inflammatory effects (such as saturated and trans fats). Healthy dietary patterns, such as the Mediterranean diet, are also associated with reduced levels of inflammatory biomarkers. Turmeric is a popular ingredient that has been shown to have anti-inflammatory effects.
How to measure the inflammatory potential of diet
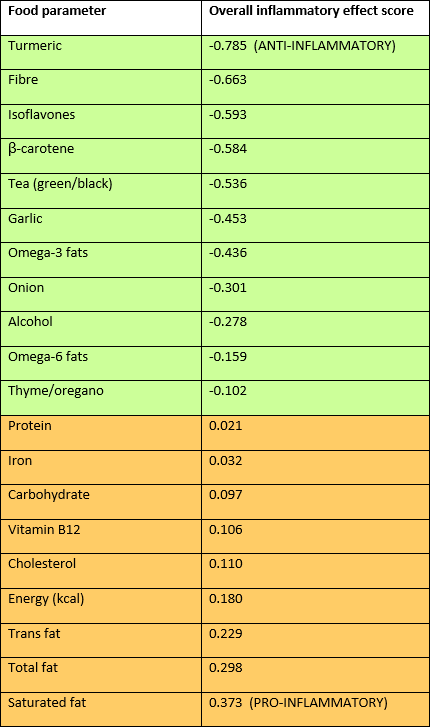
An evidence-based tool has been developed to measure the inflammatory potential of the diet called the Dietary Inflammatory Index (DII). A positive score indicates higher inflammatory potential, and scores range from -10 to 10. The tool was developed by assessing 45 food parameters and assigning a value based on the effect of the food parameter on each of six inflammatory biomarkers (IL-1β, IL-4, IL-6, IL-10, TNFα and CRP) and then weighting these according to study design and the total number of articles.
Examples of the of food parameters in the DII (source)
Does Dietary Inflammatory Index (DII) predict disease outcomes?
The evidence supporting a healthier anti-inflammatory diet for chronic disease and premature death is strong.
A meta-analysis on the association between the DII and cancer outcomes found consistent and significant positive associations between DII and cancer incidence and mortality across cancer types, study populations and study design.
A meta-analysis of the DII and cardiovascular disease (CVD) risk and mortality also found a positive association. A higher DII has been shown to be associated with reduced total mortality. Anti-inflammatory DII scores are also associated with healthier scores on other dietary indices.
Are sugars pro-inflammatory?
According to the published DII, carbohydrates generally fall into the positive numbered pro-inflammatory category, but their scores are low compared to saturated fat and total energy.
Saturated fat is almost four times more inflammatory, and total energy scores almost twice as high as carbohydrate.
There are few published studies on the DII score of different kinds of carbohydrates such as sugars versus starch, or different types of sugars and starches.
There are some studies examining associations between sugars intake and inflammatory markers. These suggest sugar-sweetened beverages (SSB) may be one factor that increases inflammation as measured by C-reactive protein (CRP): the US Health professionals follow up study in men, a US NHANES cross-sectional study in young children, a study of adults in the NHANES cohort, and a cross sectional analysis of the US Nurses’ Health Study.
Interestingly the Nurses’ Health Study found artificially sweetened beverages were also marginally associated with CRP, which suggests residual confounding, reverse causality or an ingredient apart from sugar in SSBs exerting an effect. Another analysis of the US NHANES cohort found that medium and heavy consumers of SSBs with obesity had higher CRP but there was no association in SSB drinkers who were normal weight or overweight.
A UK study that examined intakes and sources of added sugars and metabolic and inflammatory markers in a cross-sectional survey of adults found sugars from liquids were positively associated with CRP but sugars from solid foods were not associated with any outcome, whether they were natural or added.
It has been suggested that fructose may be specifically implicated in promoting inflammation, however a systematic review and meta-analysis of intervention studies on the effect of dietary sugars on biomarkers of subclinical inflammation revealed no differences in CRP between fructose and glucose, and no differences between high fructose corn syrup (HFCS) and sucrose interventions.
It may be that added sugars themselves and foods containing them are not directly pro-inflammatory, but they may displace healthful anti-inflammatory foods in the diet.
An idea supported by an intervention study that found adherence to a healthy plant-based diet reduced inflammatory factors in overweight and obese women, but less-healthy plant foods (juices, refined grains, sweet starchy food, sweets and desserts) did not increase inflammatory factors.
Obesity and inflammation
Obesity itself is a pro-inflammatory state, associated with chronic inflammation and has been termed ‘lipo-inflammation’. Weight loss reduces inflammation. For example, bariatric surgery has been shown to reduce CRP several months after surgery in adults. This association between obesity and inflammation has also been found in children, and improvement of inflammatory markers with 5% weight loss.
Associations have also been found between obesity/overweight and Dietary Inflammatory Index (DII). A cross-sectional study of 3151 university graduates in Brazil found those with the highest inflammatory potential of the diet also had the highest prevalence of overweight and obesity.
A proinflammatory diet was also associated with smoking, being sedentary and consuming an obesogenic diet (higher calories, more red and processed meats, fats and oils, fruit juices and soft drinks, sugars and sweets).
The association between dietary inflammatory index and overweight and obesity has also been found in children, with a higher DII predicting childhood overweight and obesity in an Irish longitudinal survey.
It’s difficult to disentangle the effect of dietary composition and weight status on chronic inflammation.
Importance of overall dietary pattern
Besides the anti-inflammatory effects of reduced overweight and obesity, existing research links healthier dietary patterns with reduced inflammatory potential and ultimately reduced disease risk. The overall dietary pattern is important. It is well known that healthier dietary
patterns contain fewer nutrient-poor discretionary foods and these are the most significant sources of added sugars in modern Western diets.
While consumption of added sugars is declining in Australia, the USA, Canada and the UK, dietary surveys consistently show intake of protective, anti-inflammatory plant foods such as vegetables, fruits, wholegrains, pulses/legumes and nuts are suboptimal. Strategies to increase intake of protective plant foods will likely have anti-inflammatory effects and promote health and longevity.
